(07) 5655 2156
Mon - Fri: 9am - 4pm
Sat - Sun: By Appointment
- (07) 5609 6020
Gold Coast Private Hospital
Suite 3, Ground Floor
14 Hill St, Southport Qld 4215 (Directions)
Mon - Fri: 9am - 4pm
Sat - Sun: By Appointment
Suite 3, Ground Floor
14 Hill St, Southport Qld 4215 (Directions)



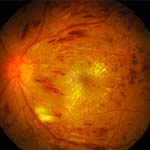
What is Diabetic Retinopathy?
Diabetes is a very common disease in our communities and can affect people of all ages including children as well as women in pregnancy. Due to the high levels of sugar in the blood, it has the ability to affect small and large blood vessels all over the body including the arteries and veins in the retina or back of the eye. Diabetes can cause these blood vessels to leak and bleed and even cause problems with the growth of new unhealthy and fragile blood vessels. This can permanently affect your vision and if left unchecked and untreated can lead to loss of your eyesight.
Symptoms of Diabetic Retinopathy
• Blurry vision
• Flashes and floaters
• Sudden loss of vision
• Wavy lines/broken lines
Treatment of Diabetic Retinopathy
The most important way to ensure healthy eyes when you are a diabetic is to have a regular eye checks, as well as control you blood sugar. Your GP, Endocrinologist and Eye specialist can all work with you to achieve this. Often specialised eye treatments are required to protect your eye sight. These may involve injections into the eye on a regular basis, laser treatment or sometimes even retinal surgery.
Regular eye checks are an important step to ensuring good eye sight when you are a diabetic. Generally, every diabetic needs at least a yearly eye check although your Doctor will discuss how frequently you need to be seen depending on the severity of your diabetes and diabetic retinopathy.
Often other tests will be required including an OCT or specialised photos of the macula and optic nerves to determine if there is any swelling or leakage that might be affecting your vision. Sometimes diabetics will also need a ‘dye test’ or Fundus Fluorescein Angiogram (FFA) where yellow dye is injected into a vein in your arm and photos of the dye travelling through the blood vessels in the back of the eye are taken.
What is Age Related Macula Degeneration (AMD)?
Age Related Macula Degeneration, often abbreviated to AMD, is unfortunately a very common degenerative eye condition which affects the macula, a small part of the retina or back of the eye. The macula is responsible for our very clear, central vision that we use all the time in our day to day activities. Therefore, when people have AMD, it can significantly impact on their quality of life due to affecting their central vision and making things like driving, recognising faces and reading difficult. Some people may notice that straight lines appear wavy or parts of words are broken or missing, this is called distortion and is common in people with AMD. If you notice any of these problems, you need to be seen by an eye specialist.
Symptoms of AMD
• Loss or blurry central vision
• Patchy vision
• Difficulty driving, recognising faces, difficulty reading
• Wavy lines/broken lines (not floaters)
Risk Factors for AMD
AMD most commonly affects people of advancing age. There are few known risk factors although we do know having a family member with this condition can put you more at risk of developing it yourself. Smoking is also known to put someone at risk of developing Macula Degeneration.
Types and Treatment of AMD
There are two main types of macula degeneration and the treatments for each are very different. Macula Degeneration is a permanent condition which cannot be cured however treatments focuses on improving or maintain quality of vision for as long as possible. Your Doctor will inform you what type you have and the most appropriate treatments.
Dry AMD is the more common type and is normally due to the deposition of unknown ‘waste’ products of the eye which leads to a weakening or atrophy of the layers of the macula. Sometimes this will even lead to permanent scarring. People with Dry AMD will often be recommended vitamin supplements and dietary improvements such as increasing their intake of oily fish, nuts and green leafy vegetables.
Wet AMD is where a blood vessel has bled and leaked into the macula region causing swelling or fluid. This may often be noticed as a sudden change or loss in your vision. Treatment of this type of macula degeneration usually involves prompt and regular injections of medications into the eye to help shrivel up the blood vessel, often every month initially. These injections have been found in very large studies to be useful in maintaining or improving vision in approximately two thirds of patients with wet AMD. Injections into the eye do not help dry Macula degeneration. Rarely, laser treatment may be recommended for some people with wet AMD.
Almost all your consultations should involve a check of your macula as part of a routine eye check. Normally a test called an OCT will assist your eye Doctor in determining the health of your macula or to monitor how you respond to treatment. Sometimes you will need a ‘dye test’ or Fundus Fluorescein Angiogram (FFA) where yellow dye is injected into a vein in your arm and photos of the dye travelling through the blood vessels in the back of the eye are taken.
Self-Monitoring of AMD
Any patient with AMD will be advised to not only have regular eye checks with their specialist but also to regularly self check their eyesight with an Amsler grid. Each eye is to tested separately, with your reading glasses on, at approximately arms length or the distance you would read a book. If there are any changes you need to contact your eye specialist immediately.