(07) 5655 2156
Mon - Fri: 9am - 4pm
Sat - Sun: By Appointment
- (07) 5609 6020
Gold Coast Private Hospital
Suite 3, Ground Floor
14 Hill St, Southport Qld 4215 (Directions)
Mon - Fri: 9am - 4pm
Sat - Sun: By Appointment
Suite 3, Ground Floor
14 Hill St, Southport Qld 4215 (Directions)




Any blockage to the tear duct area of the nasal and eye area can cause Watery Eyes.
What are the causes of watery eye?
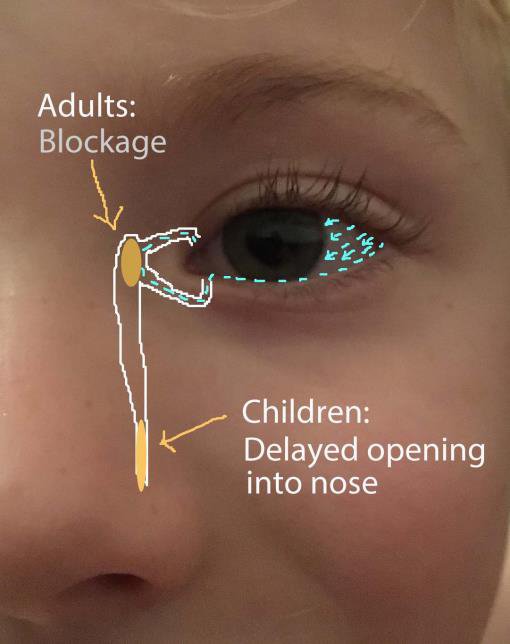
The lacrimal gland at the upper outer corner of the eyelid and orbit produces tears to lubricate and support the surface of the eye. These tears drain in the middle corner of the upper and lower eyelids in a special ‘pipe’ system that drains into the nose, called the nasolacrimal system. These ‘pipes’ start as small tubes/canals in the upper and lower lid that join together and drain into a tear sac and then down into the nose.
Watery eye (or epiphora) is caused by one of following things or a combination of these three:
1) Blockage of the nasolacrimal sac/duct causing watery eye
As an adult, the tear sac can get blocked from infections, swelling, trauma or tumours. In children, it is common for new infants to be born with a blocked tear drainage system but this normally quickly resolves itself over a few months.
1) Blockage of the nasolacrimal sac/duct causing watery eye
As an adult, the tear sac can get blocked from infections, swelling, trauma or tumours. In children, it is common for new infants to be born with a blocked tear drainage system but this normally quickly resolves itself over a few months.
What are the symptoms of this blockage?
A blocked tear/nasolacrimal sac causes watery eye, recurrent eye infections, sometimes a palpable fluctuating lump on the middle corner of the lower lid, by the nose, and occasionally marked pain over this area with increasing redness and infection of the eyelid skin that requires high doses of antibiotics or admission to hospital. In addition, the nose may feel stuffy with a history of sinus or nose problems or a past injury to this area.
How is it diagnosed?
Your Specialist will assess the tear flow drainage through to the nose using a drop of fluorescein to the eye and often will squirt some salty water into the tear duct with a fine tube/cannula to assess where the blockage is. This can occasionally be mildly uncomfortable and you will be given an eye drop of anaesthetic prior to this. For patients with nasal stuffiness or nasal symptoms, you may need examination up the nose with an endoscope. Occasionally, if there is poor flow in the tear system but no clear blockage or if the nasolacrimal system has an abnormal pattern/anatomy, you may need a special radiological scan called a Dacryocystogram. Likewise, your specialist may request a CT scan to assess for bone or sinus abnormalities of the area.
How is a blocked nasolacrimal sac/duct treated?
For adults, treatment after the acute infection stage requires a surgical bypass procedure (DCR/Dacryocystorhinostomy) of the nasolacrimal sac into the nose higher up. This can be done via a small 10-15mm cut in the skin at the side of the nose by the lower eyelid or endoscopically via the nose and may require space-creating procedures within the nose at the same time. Often a small clear rubbery tube is passed down the lacrimal system and stays in place for 6 weeks post procedure. Whilst this is in place, the full drainage of new bypass surgery will not be realized.
The success rates of surgery are extremely good. However, as the procedure requires either sedation or general anaesthetic to be performed and the patient’s cardiac status needs to be considered, it is best performed in a theatre setting, occasionally with an overnight stay.
Sometimes a full DCR is not necessary and a smaller stenting procedure may be possible to release the blockage. This is associated with a greater chance of recurrence of the watery eye.
For children, initially your Specialist will recommend firm massage or pressure with the soft part of your finger or thumb downwards over the nasolacrimal sac area and keeping the eyelids clean. If the problem persists past 12-18 months of age or if the child has recurrent severe infections, then a general anaesthetic procedure to explore and potentially open up or stent the tear duct system will be recommended.
What are the risks of nasolacrimal duct surgery?
Adult surgery has a risk of skin scar infection, bruising, failure to correct the watery eye and severe nosebleed post procedure (although usually all minimal). Because of the risk of nose bleed, it is important that you rest for the first 48 hours post surgery and avoid blood thinning agents, garlic and fish oils, if possible prior to the procedure and during this immediate post operative period. In addition, as your blood pressure needs to be lowered during the procedure, there is a risk to heart flow if you are known to have problems. Your Specialist will advise you on the best and safest way to have your procedure.
What can I expect during and after surgery?
If you opt for a local anaesthetic procedure with sedation, you will be alert during the procedure, hear sounds and see lights, but you will not feel pain. You may hear the noise when bone is removed but this is normally not distressing. Most patients tolerate a local anaesthetic procedure very well. If you prefer a general anaesthetic (fully asleep), you may feel slightly drowsier for a few days post procedure. You will need to rest for 48 hours, either way, and avoid anything that can stimulate a nosebleed. You will be given an advice sheet prior to discharge home on this. If a tube is placed during the procedure, this will need to be removed at approximately 6 weeks. This is an easy procedure in the eye clinic setting where the tube is cut and you are asked to blow your nose for it to come out. Occasionally it will need a small, in-room, retrieval from the nose. Every now and again, the clear rubbery tube will be visible or move slightly and become more noticeable in front of the eye. If it feels like it is rubbing the eye or if is causing annoyance, seek attention from your eye specialist for earlier removal – it is unlikely to affect the outcomes of your surgery.
2) Poor eyelid tone causing watery eye
Relaxed lower eyelid tone from conditions such as ectropion and facial palsy will reduce the ability of the eyelid to assist in pumping or squeezing the tears into the tear duct system to drain them away.
See the associated information sheets on these conditions.
Upper lid poor tone found in conditions such as sleep apnoea and floppy eyelid syndrome add to the problem due to compromised eye surface lubrication and comfort.
3) Compromised eye surface causing watery eye
Integrity of the eyelid margin, tone, oil production, tear film, conjunctiva and corneal surface are essential in maintaining the health of the eye surface. Conditions such as blepharitis and dry eye lead to an irritated eye surface and poor oil secretions to the tear film and thus an over production of a watery tear that evaporates quickly. This is why when faced with a cold windy day or air-conditioning, symptoms of watery eye and eye surface discomfort will worsen.
Treatment for these conditions are discussed in the Eyelid Disorder information sections.